Predicting the night-to-night variability in the severity of obstructive sleep apnea: the case of the standard error of measurement
Abstract
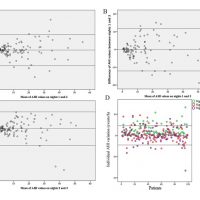
Study objectives: Night-to-night variability in the apnea-hypopnea index (AHI) may affect the accuracy of the diagnosis of obstructive sleep apnea (OSA) and treatment selection. This study was conducted to assess the utility of the standard error of measurement (SEM) in predicting the night-to-night variability in the OSA.
Methods: Ninety nine patients underwent a 3-consecutive nights of sleep monitoring with a validated home portable monitoring devise (BTI-APNiA, BTI Biotechnology Institute, Vitoria, Spain). The night-to-night variability in apnea- and hypopnea-related measures and blood desaturation were assessed. The agreement between the three nights was also assessed. The SEM and the AHI of the first night were used to calculate a range for the severity of the OSA. This range was then challenged to predict the most frequent OSA severity, the OSA severity in nights 2 and 3, and the OSA severity in the three nights.
Results: Ninety nine patients (mean age: 56±14 years) participated in the study. The mean body mass index was 25.4±4.0 Kg/m2 and the mean score of Epworth questionnaire was 8±5. The AHI of the first, second and third nights were 13.96±13.46, 13.76±12.76 and 13.52±12.91 events/h, respectively. The night-to-night variability in the AHI and the sleep time in supine position over the three nights were not statistically significant. However, the differences in the severity of the OSA was statistically significant (range of agreement in the diagnosis: 41.7%-83.3%). The standard error of measurement (SEM) considering the AHI was 4.64 events/h.. The SEM was efficient in predicting the most frequent OSA severity (among the three nights) in more than 96% of the cases.
Conclusions: The night-to-night variability in the AHI might affect the diagnosis of OSA. The use of standard error of measurement and the AHI of one single night would be of interest to predict the night-to-night variability in the severity of OSA.
Keywords: Polysomnography; Respiratory Rate.; Sleep; Sleep Apnea, Obstructive.

 English
English
 Français
Français
 Deutsch
Deutsch
 Italiano
Italiano
 Português
Português