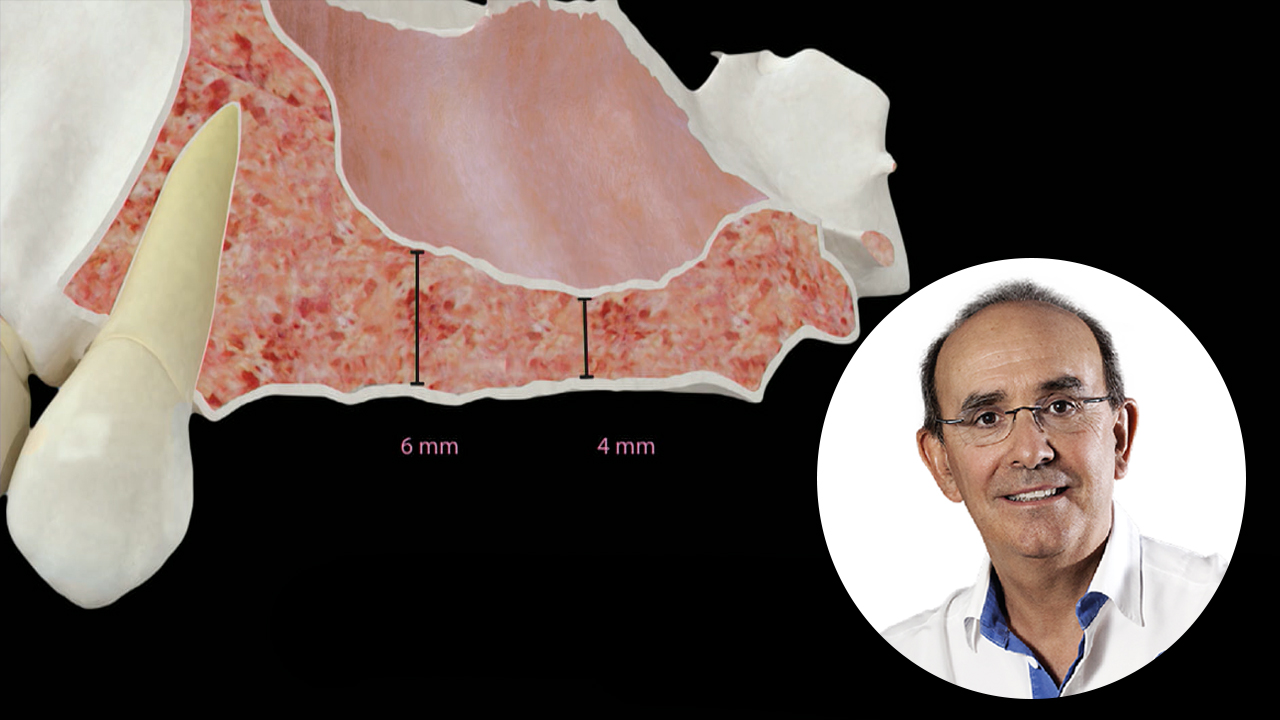
Eduardo Anitua
Doutor em Medicina e Cirurgia. Especialista em Estomatologia
Diretor do Instituto Eduardo Anitua, Instituto de investigação básica e aplicada e Centro clínico e de formação em Implantologia oral e Terapia regenerativa. Diretor científico da BTI (Biotechnology Institute).
Artigos publicados
- Autor:
- Eduardo Anitua
- Carlos Flores
- Sofía Fernández-de-Retana
- Beatriz Anitua
- Mohammad H Alkhraisat
Performance of Immediately Loaded Short Dental Implants Using Low-Speed Drilling Protocol and Plasma Rich in Growth Factors: A Controlled Retrospective Observational Study
Narrow dental implants are commonly used to restore narrow alveolar ridges. Although the good performance of narrow dental implants supporting multiple prostheses has been repeatedly demonstrated, there are few studies analyzing their performance in a long-term follow-up together with the influence of the loading protocol. Thus, the objective was to assess the influence of implant loading protocol (immediate vs delayed) on the long-term outcomes of 3.0-mm-diameter dental implants supporting fixed multiple prostheses.
- Autor:
- Eduardo Anitua
- Diez GG
- Castellanos N
- Vázquez C
- Galindo-Villardón P
- Alkhraisat MH
The effect of mindfulness on the inflammatory, psychological and biomechanical domains of adult patients with low back pain: A randomized controlled clinical trial
Narrow dental implants are commonly used to restore narrow alveolar ridges. Although the good performance of narrow dental implants supporting multiple prostheses has been repeatedly demonstrated, there are few studies analyzing their performance in a long-term follow-up together with the influence of the loading protocol. Thus, the objective was to assess the influence of implant loading protocol (immediate vs delayed) on the long-term outcomes of 3.0-mm-diameter dental implants supporting fixed multiple prostheses.
- Autor:
- Eduardo Anitua
- Asier Eguia
- Allende M
- Alkhraisat MH
Bone-Regenerative Ability of Platelet-Rich Plasma Following Sinus Augmentation with Anorganic Bovine Bone: A Systematic Review with Meta-Analysis
The objective of this systematic review is to assess the effect of the adjuvant use of platelet-rich plasma (PRP) and its type on new bone formation by anorganic bovine bone during maxillary sinus floor augmentation procedure
- Autor:
- Eduardo Anitua
- Allende M
- Alkhraisat MH
Unravelling Alveolar Bone Regeneration Ability of Platelet-Rich Plasma: A Systematic Review with Meta-Analysis
This systematic review aims to evaluate the efficacy of the available platelet-rich plasma (PRP) products and composition to regenerate alveolar bone after tooth extraction.
- Autor:
- Eduardo Anitua
- Javier Flores
- Sofia Fernandez de Retana
- Mohammad Hamdan Alkhraisat
Single-Unit Short Implants in the Molar Region: A Retrospective Study with a Minimum 3-Year Follow-up
The high biomechanical loads in molar region wounds challenge the indication for short implants to be used as a single-unit implant. This study reports on the outcomes of single-unit short implants (≤ 8.0 mm) in the maxillary and mandibular molar regions. Forty-nine short implants were placed in 48 patients to replace a missing molar tooth.
Vídeos disponíveis no BTI Channel
Para além desta pequena amostra no BTI Channel poderá expandir os seus conhecimentos em implantologia oral, medicina regenerativa e apneia do sono.

 Español
Español
 English
English
 Français
Français
 Italiano
Italiano