- Auteur:
- Eduardo Anitua
- Joaquín Durán-Cantolla
- Mohammad H. Alkhraisat
- Rafael Crovetto-Martínez
- Miguel Crovetto
- Antonio Municio
- Ramón Kutz
- Felipe Aizpuru
- Erika Miranda
Efficacy of mandibular advancement device in the treatment of obstructive sleep apnea syndrome: A randomized controlled crossover clinical trial
Abstract
Background: Evaluation of the efficacy and safety of a mandibular advancement device (MAD) (KlearwayTM) in the treatment of mild-to-moderate obstructive sleep apnea and chronic roncopathy.
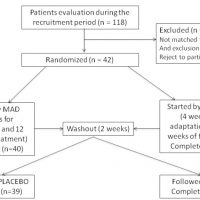
Material and methods: A randomized, placebo-controlled, double blinded, and crossover clinical trial was conducted. Placebo device (PD) defined as a splint in the centric occlusion that did not induce a mandibular advancement served as a control. The mandible was advanced to the maximum tolerable distance or to a minimum of 65% of the maximum protrusion. After each sequence of treatment, patients were assessed by questionnaires, conventional polysomnography, and objective measurement of snoring at the patient’s own home.
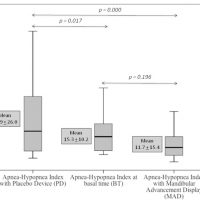
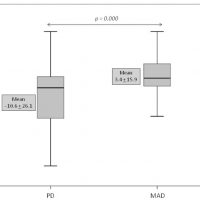
Results: Forty two patients participated in the study and 38 completed the study. Patients mean age was 46 ±9 years and the 79% were males. The mean mandibular advancement was 8.6 ±2.8 mm. Patients used the MAD and the PD for 6.4 +2.4 hours and 6.2 +2.0 hours, respectively. Secondary effects (mostly mild) occurred in the 85.7% and the 86.8% of the users of MAD and PD, respectively. The MAD induced a decrease in the apnea-hypopnea index (AHI) from 15.3 +10.2 to 11.9 +15.5. The 50% reduction in the AHI was achieved in the 46.2% and the 18.4% of the patients treated with MAD and PD, respectively. The use of the MAD induced a reduction in the AHI by 3.4 +15.9 while the PD induced an increase by 10.6 +26.1. The subjective evaluation of the roncopathy indicated an improvement by the MAD and an increase in the perceptive quality of sleep. However, the objective evaluation of the roncopathy did not show significant improvements.
Conclusions: The use of MAD is efficient to reduce the AHI and improve subjectively the roncopathy. MAD could be considered in the treatment of mild-to-moderate OSA and chronic roncopathy.

 Español
Español
 English
English
 Italiano
Italiano
 Português
Português